8 mins read
Why No Periods Is A Cause For Concern

- Menstrual Cycle As A Barometer Of Healthy Hormones
- What Is Amenorrhea?
- Causes Of Amenorrhea
- 2. Hypothalamus Or Pituitary Gland Problems
- 3. Problems With Reproductive Organs
For many women, having a monthly period is at best an inconvenience and at worst causes unpleasant symptoms such as stomach cramps, mood changes and headaches. So, missing a few periods can initially seem like a freeing experience, but it’s actually a sign something is wrong with your hormone network.
In this blog, we take a look at the role periods play in women’s hormone health and why not having a period is a sign of a hormone imbalance. We look at the causes, symptoms and treatments of no periods, a condition called amenorrhea.
Menstrual Cycle As A Barometer Of Healthy Hormones
The four key female hormones – follicle-stimulating hormone, luteinising hormone, oestrogen, and progesterone – have an intricate and complex interplay across a woman’s menstrual cycle.
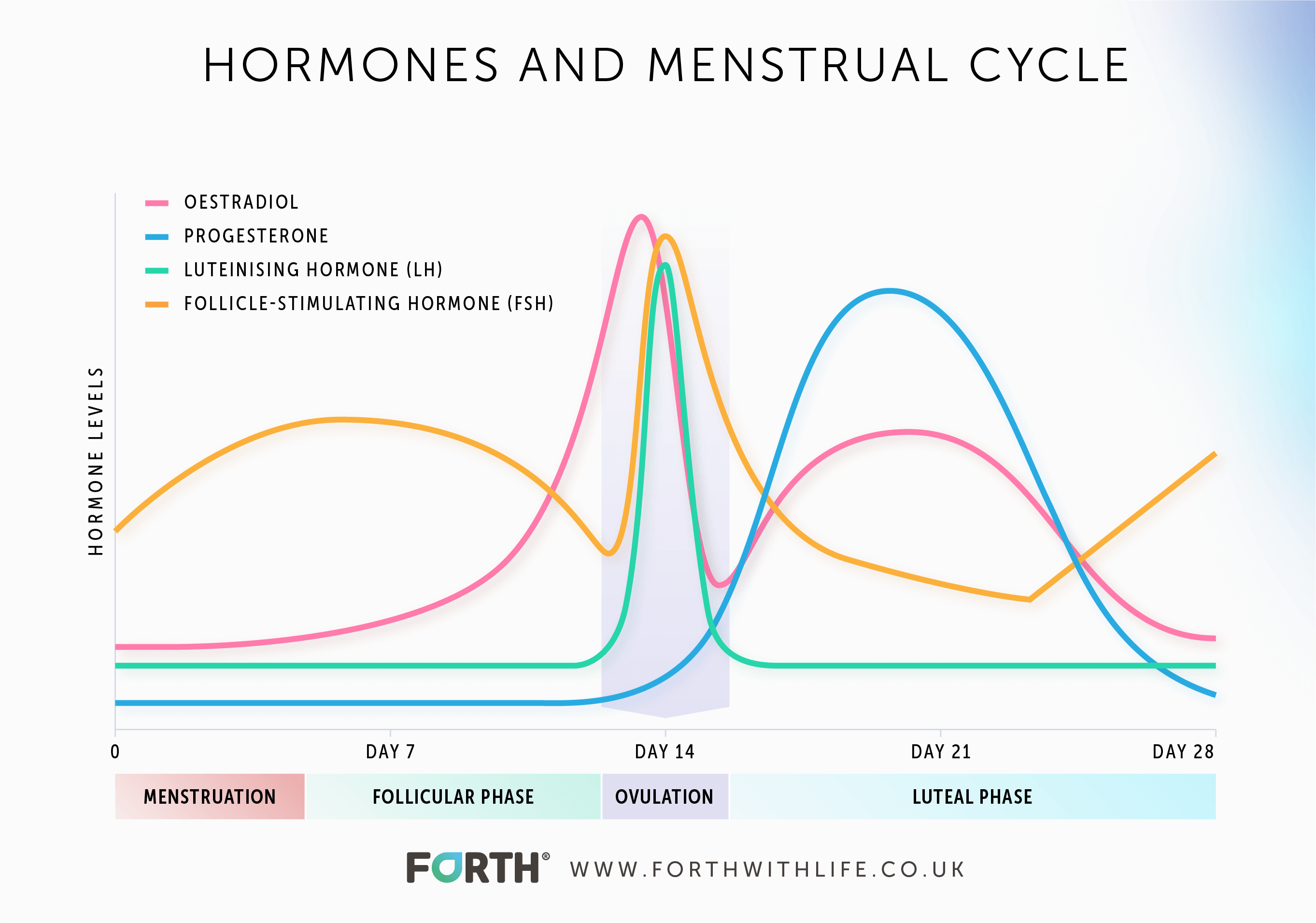
These hormones rise a fall naturally through each phase of the menstrual cycle in order to prepare the body for pregnancy. If there is no pregnancy, then menstruation occurs and the whole cycle starts again.
If menstruation doesn’t occur – and you aren’t pregnant or perimenopausal – then it’s a sign that this finely tuned hormone network is not working as it should.
Learn more about the menstrual cycle.
If you miss three or more periods in a row it is defined as amenorrhea.
What Is Amenorrhea?
Amenorrhea is the term used to describe a lack of periods in women of reproductive age. As mentioned above, it’s defined as missing three or more periods in a row rather than missing the odd period every now and again.
There are two types of amenorrhea:
- Primary Amenorrhea is when a woman reaches the age of 15 without starting her first period.
- Secondary Amenorrhea is when a woman of reproductive age stops having regular periods.
Causes Of Amenorrhea
Primary Amenorrhea Causes
If a woman has not had her first period by the age of 15, then the possible causes include[i]:
1. Ovarian Failure
This can include a chromosome disorder or genetic problems with the ovaries[ii]. If the ovaries are not functioning correctly, it will impact the release of the two ovarian response hormones – oestrogen and progesterone – and the release of an egg from the ovaries (ovulation). This will not only impact a woman’s fertility but her overall wellbeing as oestrogen plays such as wide-ranging role in a woman’s body.
2. Hypothalamus Or Pituitary Gland Problems
This is often referred to as Hypothalamic Amenorrhea. The hypothalamus is a part of the brain that plays a role in the release of hormones from the pituitary gland. So, an issue with either of these will cause a hormone imbalance and therefore affect the menstrual cycle.
3. Problems With Reproductive Organs
This is when the reproductive organs have not developed properly, and parts of the reproductive system are missing.
Secondary Amenorrhea Causes
There are natural causes of secondary amenorrhea such as pregnancy and menopause. Then there are the more obvious reasons for no periods such as taking hormonal contraception. Women can also suffer from amenorrhea when they come off hormonal contraception as their natural hormone fluctuations return to normal – which can take 2-4 weeks. If a woman’s period has not returned within 3 months of coming off hormonal contraception, she should visit her GP.
Learn more about coming off hormonal contraception.
Main causes of secondary amenorrhea:
- Pregnancy
- Breastfeeding
- Menopause
- Birth control
- Cancer treatments
- Certain prescription medications such as antidepressants, antipsychotics, blood pressure and allergy medications [iii].
- Lifestyle
- Conditions related to female hormones
Assuming all other causes have been ruled out, the next step is to look at your lifestyle and investigate conditions related to female hormones.
Lifestyle And Secondary Amenorrhea
Your lifestyle can have a big impact on your hormone health. Stress from work or family life, poor sleep, poor diet, too much or too little exercise, being under or overweight all have an impact on your hormones causing a hormone imbalance.
Our bodies and hormones work in tune with 4 biological clocks or biochronometers:
- The diurnal cycle is based on every 24 hours as a result of the full rotation of the Earth.
- The circadian rhythm is based roughly on every 24-25 hours depending on light/dark cycles, so can vary slightly according to the season.
- The infradian cycle runs over more than a day, for example, the lunar month of the menstrual cycle.
- And lifespan time is the longest in chronobiology.
The menstrual cycle is on an infradian rhythm. Our levels of the hormone cortisol are tuned into the diurnal rhythm. Our sleep/wake cycle is tuned into the circadian rhythm as are our other hormones including FSH, LH and growth hormones – all key to the development of the reproductive system and the menstrual cycle.
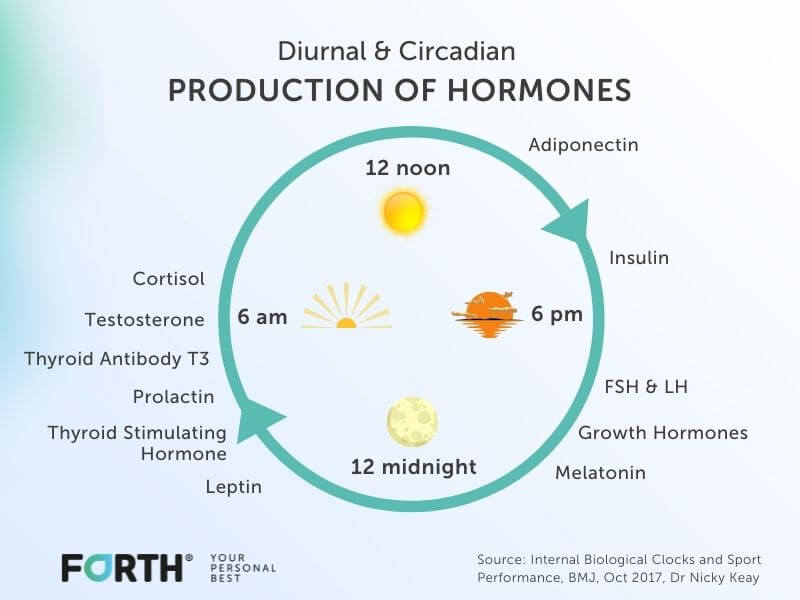
A well-balanced lifestyle that incorporates a good work/life balance, good diet, restful sleep, and the right amount of exercise will keep the body’s biochronometers in balance and therefore your hormone network too.
In contrast, doing too much exercise, not eating enough calories to fuel your activity (including unplanned exercise such as housework or playing with the kids), and not resting enough will impact your body’s biological clocks and have an impact on its hormone network.
Poor Sleep
Not getting enough sleep or poor-quality sleep will impact your circadian rhythm which in turn will impact the production of hormones such as FSH and LH. Low levels of these two control hormones will impact the release of the ovarian response hormones – oestrogen and progesterone. This will result in irregular or missed periods.
Poor Diet
Not eating enough food or the right foods to fuel your body causes it to seek fuel from other areas of the body.
In extreme circumstances such as over-exercising and under-fuelling or in people with eating disorders like anorexia, this can lead the body to shut down functions that are non-essential to life – this includes the menstrual cycle.
It’s not uncommon for female athletes to suffer from secondary amenorrhea caused by over-training and under-fuelling leading to a condition called Relative Energy Deficiency in Sport or RED-S.

But it’s not just female athletes that can suffer from this, women who are not eating enough compared to the amount of activity they are doing can also put themselves at risk of developing RED-S.
Conditions That Cause Secondary Amenorrhea
There are a number of conditions related to female hormones that cause secondary amenorrhea, these include PCOS and primary ovarian insufficiency which is when a woman experiences menopause before the age of 40.
Adrenal gland disorders and conditions that affect the thyroid such as hypothyroidism can cause secondary amenorrhea.
Amenorrhea Symptoms
The specific symptoms that accompany amenorrhea will depend on the underlying cause. For example, symptoms of PCOS also include increased facial hair, rapid weight increase or loss, acne, and depression. Symptoms of hypothyroidism include fatigue, sensitivity to the cold, constipation, slow movements and thoughts, muscle weakness and aches.
All of these symptoms are related to a hormonal imbalance which and also include:
- anxiety
- blurred vision
- digestive issues, constipation, or diarrhoea
- difficulty concentrating and memory problems
- mood changes
- dry skin or oily skin
- excess hair growth (hirsutism)
- fertility issues
- frequent peeing
- increased thirst
- hair loss
- heart palpitations
- intolerance to the cold or heat
- low sex drive
- muscle weakness, cramps, aches
- pins and needles
- slow heartbeat
- sweating
- tiredness
- weight gain or loss
Treatment Of Secondary Amenorrhea
Treatment very much depends on the cause. If secondary amenorrhea is caused by lifestyle factors, then changing these will help rebalance your hormone network and your periods will return.
If the cause is due to a condition, then in certain cases medication will be prescribed to address the hormonal imbalance and your periods should return.
Recovering From Amenorrhea
The sign that your hormones are returning to their normal fluctuations is the arrival of your first period after amenorrhea.
For women suffering from amenorrhea getting their first and second period can be overwhelming as they get that much needed confirmation that the changes they’ve made are working.
Once your periods have returned, it’s important to monitor your hormone fluctuations to find out how quickly you are recovering. It can be easy to think everything is back to normal, especially if you feel well. And if your amenorrhea was caused by over-training and under-fuelling it can be all too tempting to get back to training too soon.
One way to monitor your hormone health is by tracking your levels of FSH, LH, oestrogen, and progesterone across your entire menstrual cycle. This will show how your control hormones are interacting with your ovarian response hormones and if the rise and fall across your menstrual cycle are at the right levels.
Our innovative advanced female hormone test, MyFORM™, is an easy way to get this insight. From just two blood samples taken on day 14 and day 21 of your cycle, it can predict your hormone fluctuations across your entire menstrual cycle. You will not only receive individual results for each hormone but a map of your hormone curves across your cycle and a personalised report from endocrinology expert Dr Nicky Keay.
Summary
Not having a period for more than 3 months is a clear sign something is up with your hormone network. Amenorrhea is a condition that must be looked into as soon as possible to identify the underlying cause of a lack of periods. This can be due to a number of factors such as lifestyle, diet, medication or conditions related to female hormones.
Understanding how your hormones fluctuate across your entire menstrual cycle is key to monitoring any conditions related to your female hormone network.
This information has been medically reviewed by Dr Nicky Keay
Nicola has extensive clinical and research experience in the fields of endocrinology and sport and exercise medicine. Nicky is a member of the Royal College of Physicians, Honorary Fellow in the Department of Sport and Exercise Sciences at Durham University and former Research Fellow at St. Thomas' Hospital.

Dr Nicky Keay
BA, MA (Cantab), MB, BChir, MRCP.
Related articles
Like this article? Here are some more based on similar topics.




