6 mins read
Is Hormonal Contraception Masking Underlying Female Hormone Issues?
Author: Forth
August 10, 2021
Female health

Hormonal contraception is a reliable method to prevent pregnancy, but it can also be prescribed to women to ease symptoms that could be related to female health problems such as PCOS or endometriosis.
We take a look at how prescribing hormonal contraception could be masking underlying female hormone issues.
What Is Hormonal Contraception?
Hormonal birth control methods contain synthetic versions of the female hormones, progesterone and oestrogen, either in combination or progesterone-only.
There are several different methods of hormonal contraception and finding the best type for you will depend on your lifestyle. All types of hormonal birth control work to prevent pregnancy.
These are the different hormonal contraception types:
- The combined oral contraceptive pill (the pill)
- The progesterone-only pill (mini-pill)
- The implant
- The intrauterine system
- Contraceptive injection
- Vaginal ring
- Contraceptive patch [1]
What Impact Does Hormonal Contraception Have on Women’s Bodies?
Women’s hormones naturally fluctuate across their menstrual cycle, rising and falling through each phase.
The four main hormones involved in the menstrual cycle are the two control hormones follicle-stimulating hormone and luteinising hormone, and the two ovarian response hormones oestrogen and progesterone.
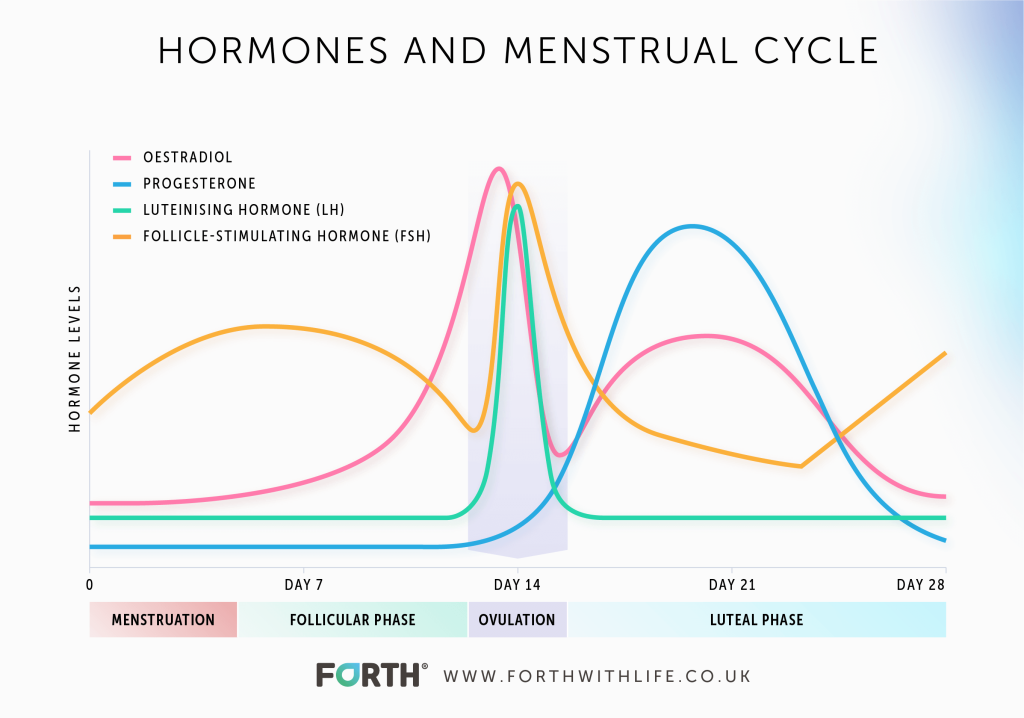
When a woman takes a hormonal contraceptive, these natural fluctuations are changed in order to prevent pregnancy.
This is a result of the way hormonal contraceptives work. They use artificial versions of Oestrogen and/or Progesterone which suppress the release of FSH and LH which are required to trigger ovulation around day 14 and ‘restarting the cycle after a menstrual bleed. [4]
Therefore, hormonal contraceptives prevent the natural menstrual cycle by maintaining consistent levels of Oestrogen and/or Progesterone to prevent ovulation, thickening the cervical mucus to stop sperm from entering the womb and fertilising an egg; as well as thinning the lining of the womb to lower the chances of a fertilised egg implanting and developing.
The combined oral contraceptive pill mimics a natural menstrual cycle as it’s taken daily for 3 weeks followed by a week of no pills. This causes what’s known as a withdrawal bleed or ‘break-through bleeding’ due to the drop in hormones.
Although it may seem a woman is having a ‘normal’ menstrual cycle, the high levels of Oestrogen and Progesterone prevent the natural menstrual cycle that underpins ovulation [4].
Essentially, hormonal contraceptives cause a hormone imbalance in women to prevent them from becoming pregnant.
How Does Female Hormonal Contraception Mask Health Issues?
The menstrual cycle is a barometer of a healthy endocrine system. By taking a hormonal contraceptive any changes to a woman’s hormones will go unnoticed until she comes off the contraception.
This was the case with Issy Morris, an elite triathlete who didn’t realise she was suffering from a condition known as Relative Energy Deficiency In Sport (RED-S).

RED-S is caused by over-training combined with under-fuelling, so the body shuts down secondary functions to focus on primary functions essential for life maintenance. In women, this can cause periods to stop.
It wasn’t until Issy came off her contraceptive and her periods didn’t return that a diagnosis of RED-S was finally confirmed. If she hadn’t decided to stop her contraception, she wouldn’t have known.
A year on and Issy is still recovering. She otherwise feels fine, but by tracking her hormones using our advanced female hormone test, MyFORM™, she can see that her hormone fluctuations are not yet back to normal, so she is unable to return to training. Without this insight, Issy would’ve started training too soon causing further issues with her hormone health.
But it’s not just sportswomen that this affects. Women are often prescribed hormonal contraception to manage symptoms related to their hormones. However, if a woman’s period is irregular, unusually heavy, or painful then it’s a sign that something is wrong and further investigation is needed.
Far too often women are prescribed hormonal contraception to manage these symptoms when they are in fact a sign that there could be a health issue such as endometriosis, functional hypothalamic amenorrhoea, or polycystic ovary syndrome.
Although hormonal contraception like the combined pill, is sometimes used to manage certain conditions like polycystic ovary syndrome and endometriosis [5], there are certain conditions where its use is not advised.
Functional hypothalamic amenorrhoea (FHA) is a condition that is associated with weight loss, exercise or stress and leads to metabolic and hormonal issues. A consequence of this is the hypothalamus doesn’t release enough GnRH and causes periods to stop [6]. The Endocrine Society advises against using oral contraceptive pills to treat FHA to help regain regular periods or for improving bone mineral density [6].
It is also important to establish the underlying cause of changes to a woman’s menstrual cycle so that the correct treatment can be prescribed.
Being given hormonal contraception without ruling out other conditions related to female hormones could result in a woman experiencing long term fertility issues as well as poor health.
How Do You Know If Your Contraception Is Masking A Health Issue?
In the first instance, you should only choose to use hormonal birth control if you have regular periods or if the cause of irregular or painful periods has been diagnosed.
If you have been prescribed hormonal contraception to manage irregular or heavy periods, then you may want to gain advice from an endocrinologist to help rule out any health conditions that may be impacting your hormones.
If you are concerned, you may want to consider coming off hormonal contraception and using other barrier methods of contraception. That way you can allow your hormones to return to their natural state and see if your periods are normal for you.
You can also use our MyFORM™ product once your periods have returned to map all 4 key female hormones across your entire menstrual cycle. This will give you in-depth detail on the health of your hormone network and by logging symptoms at the time of doing the test, we can correlate any symptoms to your hormone fluctuations.
Learn more by reading our blog ‘What Is MyFORM™?’.
Conclusion
Hormonal contraception should only be prescribed to women having regular periods. It should not be prescribed to manage symptoms such as heavy, painful, or irregular periods without other conditions being ruled out first.
- Health scores calculated
Close
Article references
-
Gordon, C, M et al. Functional Hypothalamic Amenorrhoea: An Endocrine Society Clinical Practice Guideline. JCEM 102(5), PP 1413-1439.
This information has been medically reviewed by Dr Nicky Keay
Nicola has extensive clinical and research experience in the fields of endocrinology and sport and exercise medicine. Nicky is a member of the Royal College of Physicians, Honorary Fellow in the Department of Sport and Exercise Sciences at Durham University and former Research Fellow at St. Thomas' Hospital.

Dr Nicky Keay
BA, MA (Cantab), MB, BChir, MRCP.
Related articles
Like this article? Here are some more based on similar topics.